This article shares personal experiences and is for informational purposes only. It is not career or medical advice.
TL;DR – Understanding the Healthier SG Scheme
- Healthier SG funds your first preventive check-in (age 40+ citizens/PRs) + subsidised screenings & vaccinations.
- Chronic meds ordered via Alps are capped at polyclinic prices — big savings for multiple prescriptions.
- Private GPs get some support but fixed margins & grants remain small compared to rising rents & wages.
- It bridges cost gaps but doesn’t fully solve post-COVID expense pressures on private clinics.
In the second episode of Uncle Talks Podcast, three Singapore doctors— Dr Kenneth Tan (a private general practitioner), Dr John Hsiang (private gastroenterologist), and Dr Leong Choon Kit (veteran family physician) turned their attention to one of the most talked-about changes in primary care: the Healthier SG scheme.
What began as a casual discussion about rising healthcare costs quickly became a candid exploration of how this government initiative is attempting to reshape the landscape for both patients and private clinics in Singapore.
Their conversation revealed not just the mechanics of the programme, but the real-world tensions, small victories, and ongoing negotiations that define its rollout in 2026.
The doctors did not shy away from the scheme’s complexity. They described it as having “many limbs,” with preventive health and chronic disease management forming its backbone.
For patients above 40 who are citizens or permanent residents, the programme funds an initial health check-in with a private GP, opening the door to subsidised screenings, vaccinations, and lifestyle counselling.
One of the doctors explained that this preventive focus has already driven noticeable uptake: “There was a large uptake in terms of influenza vaccinations, pneumococcal vaccinations among our older patients.”
What makes this meaningful, they emphasised, is the shift toward earlier intervention. Instead of waiting for chronic conditions to worsen, patients now receive structured support to manage risk factors—weight, blood pressure, smoking, exercise, diet—before problems escalate.
The scheme does not simply subsidise treatment; it tries to keep people healthier for longer, a goal that resonates deeply with primary care physicians who see preventable disease every day.
Preventive Health: Catching Problems Before They Grow
The preventive arm of Healthier SG stands out as one of its clearest wins for patients. By funding that first comprehensive check-in, the programme encourages people who might otherwise delay seeing a doctor to come in early.
The doctors noted that this single funded consultation has prompted many to complete overdue health screenings and vaccinations—steps that can dramatically reduce future hospitalisations and costs.
For clinics, the benefit is twofold. First, it brings patients through the door who might not have come otherwise.
Second, it allows GPs to build longer-term relationships from the outset. One doctor observed that the scheme’s emphasis on risk-factor analysis—measuring BMI, discussing diet and exercise, offering smoking cessation support—gives clinics a structured way to deliver meaningful preventive care rather than simply reacting to illness.
Yet the doctors were realistic: while the preventive component is valuable, it addresses only part of the broader cost pressures facing private practices.
Chronic Care Subsidies: A Partial Bridge Over Rising Costs
The scheme’s second major pillar—chronic disease management—attempts to ease the financial burden for patients on long-term medications. Private GPs enrolled in Healthier SG can now order subsidised drugs through a central purchaser called Alps.
The price charged to patients is capped at levels comparable to polyclinics, and subsidies are further adjusted based on income tiers (CHAS Blue, Orange, Green, PG, MG).
This mechanism, the doctors explained, offers genuine relief for patients managing multiple chronic conditions. “Patients are assured that the amount that they are paying is comparable to that at the polyclinic for their medications,” one noted.
For many, especially those on fixed incomes, the difference between polyclinic and private clinic drug prices had previously been a barrier to consistent care.
For clinics, however, the picture is more nuanced. While patients benefit from capped prices, the doctors pointed out that the margin on these subsidised drugs remains fixed and often slim. “The margin is fixed,” one remarked, “but of course that benefits the patient.”
The Chronic Enrolment Grant, intended to offset some of the financial impact on clinics, was described as “still very small compared to what they could have lost.”
Several of the doctors mentioned ongoing discussions with the Ministry of Health to refine the scheme, suggesting that while Healthier SG is a step forward, it remains a work in progress.
The Business Reality: Private Clinics Navigate a Tight Margin World
The conversation repeatedly circled back to a central tension: private primary care operates as a commercial enterprise without the institutional funding enjoyed by polyclinics or public hospitals.
Rising rents, manpower costs, and inflation have placed enormous pressure on GPs, especially since COVID. One doctor described some new HDB clinic spaces commanding rents as high as $52,000 per month for just 500–600 square feet—an almost unimaginable figure for many.
In this environment, Healthier SG’s subsidies for chronic drugs provide partial relief but do not address the full spectrum of rising expenses.
The doctors were frank about the trade-offs: some clinics upscale their services and charge higher consultation fees to remain viable, while others rely on volume and efficiency. “Different strokes for different GPs and really different patients,” one observed, noting that patients ultimately decide where to go based on their own priorities—cost, convenience, trust, or perceived quality.
What emerged clearly was a shared commitment to patient care despite these pressures. The doctors repeatedly returned to the idea that their role is to help patients navigate the system, whether that means guiding them toward subsidised routes, explaining insurance limitations, or simply being transparent about costs.
One summed it up: “At the end of the day we all doctors, we all try to help our patients.”
What This Means for Patients and the Future of Primary Care
For patients, Healthier SG offers tangible benefits—funded preventive check-ins, subsidised chronic medications, and greater emphasis on early intervention—that can make staying healthy more affordable and accessible.
For private clinics, the scheme provides a framework to retain patients who might otherwise drift toward polyclinics, while also aligning financial incentives with preventive and chronic care.
Yet the doctors made no secret of the scheme’s limitations. It does not fully offset the post-COVID cost pressures, and many questions remain about long-term sustainability for private primary care.
The conversation ended on a note of cautious optimism: Healthier SG is an evolving initiative, shaped by ongoing dialogue between the Ministry and the GP community. Its success, they implied, will depend on whether it can continue to balance patient affordability with the economic realities of running a private clinic.
In a healthcare system where costs are rising faster than many incomes, programmes like Healthier SG represent an important attempt to keep primary care within reach.
For patients over 40, the message is straightforward: enrol, get that funded check-in, and take advantage of the preventive and chronic care subsidies.
For private GPs, it is a partial lifeline—one that helps, but does not eliminate, the daily challenge of balancing quality care with financial survival.
As one doctor put it toward the end: “It is difficult when you have rising cost, rising rental and you’re trying to keep everything if you’re trying to keep healthcare as effective as before but you’re trying to keep the cost down.”
That tension, more than any single benefit, may define the true story of Healthier SG in the years ahead.
Want to hear more about the doctor’s opinion on healthcare in Singapore? Listen to the original Uncle Talks Podcast.
FAQ – Understanding the Healthier SG Scheme
1) Who can benefit from Healthier SG preventive services?
Citizens and PRs aged 40 and above. It funds your first comprehensive health check-in with an enrolled private GP, plus subsidised screenings and vaccinations (e.g., flu, pneumococcal).
2) How does Healthier SG make chronic medications cheaper in private clinics?
Enrolled GPs order subsidised drugs from Alps. The price you pay is capped at polyclinic levels, with further subsidies based on your CHAS card/income tier.
3) Do private clinics receive subsidies under Healthier SG?
Not directly for consultations. They receive a small Chronic Enrolment Grant based on the number of enrolled chronic patients, but many doctors say it’s still too low to offset rising rents and wages.
4) Has Healthier SG increased vaccinations among older patients?
Yes — doctors have seen a large uptake in influenza and pneumococcal vaccinations since the scheme started funding preventive care.
5) Why do private GPs say Healthier SG margins are tight?
They must sell subsidised drugs at fixed (polyclinic-level) prices, so profit margins are capped. The grant helps a little, but doesn’t fully cover post-COVID increases in rental and manpower costs.
6) Should patients enrol in Healthier SG if they already use polyclinics?
If you prefer seeing a private GP for convenience or continuity, yes — you can get similar subsidised chronic drug prices and funded preventive checks without switching entirely to polyclinics.
About the Expert
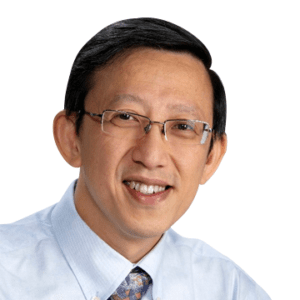
Dr Leong Choon Kit
MBBS, M.Med (Public Health), GDFM, MCFP(S), FCFP(S), FAMS(Family Medicine)
Dr. Leong Choon Kit is one of the Doctors at MMC. A dedicated physician with a background in Public Health and Family Medicine, focusing on public policy, social issues, and vaccination advocacy.
About the Writer
Timothy Leong
Timothy Leong is the writer, content editor and marketing specialist at MMC. With experience in writing and creating websites for local businesses. Basically makes sure that everything online runs smoothly.



